The Unrelenting Zebra
Jenise Finlay had to dedicate her life to medicine to get the care she needed to diagnose and support her invisible disability.
Jenise is an advanced practitioner nurse and PHD student at the University of Victoria with chronic pain that results from an invisible disability called Ehler’s-Danlos Syndrome.
Due to a lack of understanding into women’s chronic pain, Jenise did not get diagnosed with Ehler's-Danlos Syndrome until 2021, at the age of 29.
Jenise had been looking for a diagnoses for her chronic pain since the first onset of debilitating muscle pain starting in her lower legs at age 14.
Ehler’s-Danlos Syndrome does not have a cure.
Content Warning
Video may be graphic to some viewers. Viewer discretion is advised.
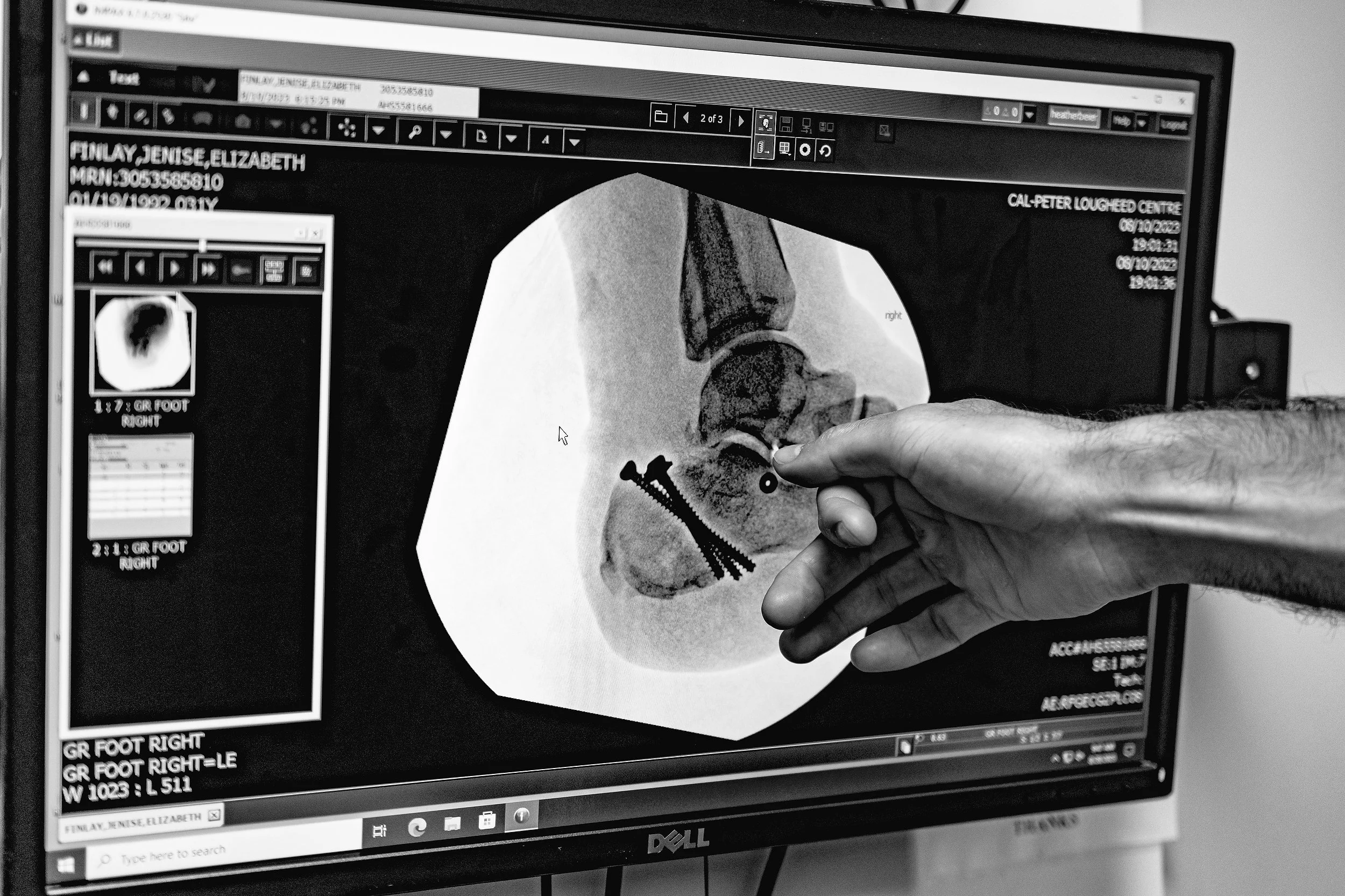
Jenise Finlay took a 30 foot fall while rock climbing sustaining a break to her heel in a tongue-type fracture with a secondary fracture in the sublateral joint.
Ehler’s-Danlos syndrome prevents Jenise from healing at the rate of a healthy person who does not have EDS.
“falls are really scary for me with Ehler’s-Danlos Syndrome because healing is impaired. If I tear something or I break something, it may never go back to normal. So I may never make a full recovery.”
“When you have lost so much already, it's really hard to lose the things you've held on to. I've had to give up so much in my life because of how my body is with Ehler’s-Danlos Syndrome, it doesn't work properly.”
Finlay relies on physiotherapy and connective tissue strengthening exercises to prevent injuries caused by her hyper-mobility. Jenise is cognizant of her body at all times because her movements could cause an accidental injury.
Despite doctors telling Finlay to stop climbing due to high risk of injury, Jenise has found rock climbing as an aid in her symptom management of EDS and is reliant on the activity for the benefits it brings to her mental and physical well-being.
Jenise said, “When I'm not able to be active, everything is deconditioned and then I'm much more prone to dislocation of my joints, and my joints aren't supported by my connective tissue anymore. My pain is worse.”
According to the Ehler’s-Danlos Society 1 in 5000 people may have EDS.
Excerpt from Emerging Adult Women with Chronic Pain: A Narrative Inquiry
by Jenise Finlay
Women are disproportionately affected by chronic pain, yet women’s pain is frequently discounted or underestimated by medical professionals.
Emerging adult women are at higher risk for insufficient pain management and face unique challenges navigating chronic illness, dating, body image, college, careers, establishing independence from family, and bearing children at an age where youth is equated to being healthy.
An increasing prevalence in chronic pain has been observed across all age groups in Canada, most notably among those aged 20 to 29 with no other health conditions, yet few qualitative studies examine chronic pain exclusively in women under 30.
By being able to bridge the gap between the medical system and patient care, Jenise was able to work in her field while conducting research into her well-being, diagnosis, and symptom management.
“Women’s chronic pain is dismissed in the healthcare system.” said Jenise Finlay, advanced practice nurse.
“Chronic pain is not just dismissed within healthcare, but women themselves learn to dismiss their own pain by having to engage in a system that is inadequate at managing the complexity of chronic pain disorders.”
It is nearly impossible to advocate as a patient as the misconceptions surrounding chronic pain in women makes the health care they have access to defective.
Women in chronic pain cannot always access private healthcare and specialists to diagnose and treat their pain.
According to “It’s All in Your Head”: A Meta-Synthesis of Qualitative Research About Disenfranchising Talk Experienced by Female Patients with Chronic Overlapping Pain conditions.
“COPCs’ status today can be compared historically to research on the experiences of patients living with HIV/AIDS in which medical professionals were perceived early on as being “not uniformly knowledgeable about the disease nor uniformly unbiased in their attitudes toward those who need care” (Metts & Manns, 1996,
Without proper care, chronic pain decreases quality of life and leaves women in a cycle of intuitively knowing there is something wrong but not being able to get diagnosed.
A lack of a diagnose can leave women questioning themselves and hesitant to seek out help for their chronic pain.
This leads to self isolation, decreased body image, and can prevent them from having a life worth living because of the barriers that they face to participate in society.
Finlay said, “You face stigma not just from the system but also your friends and family which is really hard if you don’t have a supportive family or friend group.”
Women in chronic pain have to live in pain with no support outside of their friends and family, there is no government subsidies for women with chronic pain.
Untreated and undiagnosed chronic pain can lead to increased health issues as the cycle they face is endless and can lead to feelings of hopelessness.